What Is Death?
An excerpt from 'The Future Loves You'
The following is an excerpt from my new book, ‘The Future Loves You: How and Why We Should Abolish Death’. Available now in hardcover, audiobook, eBook.
In the past few decades, medical science has rendered obsolete centuries of experience, tradition, and language about our mortality and created a new difficulty for mankind: how to die.
Atul Gawande, Being Mortal
Even if Trent's skull didn't break when he initially hit the concrete, it certainly did once the trailer fell on top of him. One second he was relishing the thrill of being pulled along behind a dune buggy, the next he was unconscious with his skull fractured in seven places. Following the injury he was rushed to hospital, where doctors began desperately trying to put his head back together. Half the task was just keeping him alive while they did so. Over several days of surgery his heart stopped four times, with more and more damage accumulating to Trent’s body with each pause. Disappointingly, at the end of all this, though his skull was patched, he was yet to show any signs of consciousness.
The medical team decided continuing treatment at this stage would simply be forestalling closure for his family, as he had vanishingly little hope of recovery. His mother wearily agreed that her son shouldn’t be left like this. She knew her son was generous, and that he would have wanted to donate his organs to help others with lives that could still be saved. However, with his heart still beating, Trent wasn’t officially dead yet. Even though it had been several days and four cardiac arrests since he hit the concrete, there was one additional test the medical team needed to do before Trent could be declared dead: a final brain scan.1,2
Trent’s story is a lot more complicated than it would have been a century ago. Back then, Trent would have been considered dead the first time his heart stopped, at the latest. In general, before the middle of the twentieth century diagnosing death was clear cut – alive if lungs breathing and heart beating, dead otherwise.[1] These days, determining when exactly someone dies is a lot murkier.
The first major complication came with the invention of mechanical ventilators, which blurred the link between breathing and life.[2] These devices could artificially inflate a patient’s lungs if they stopped breathing on their own, and were initially invented to assist with respiratory failure during surgery.[3] Next came cardiopulmonary bypass machines, unseating the heart as the determinant of life by artificially circulating a person’s blood. Using a series of pumps and tubes, someone could now have their heart stopped, operated upon, potentially even replaced with a transplant from another person, all without being considered dead. These days a person can be kept alive for weeks with neither functioning heart nor lungs using a technique called extracorporeal membrane oxygenation. This method involves draining a patient’s blood into tubes, passing it through an artificial lung that introduces oxygen and removes carbon dioxide, then pumping the blood back into their body. Through these processes, death and the cardiorespiratory organs have been completely decoupled.
These once unimaginably futuristic technologies have severed the definition of death from its origins and set it adrift. Where it will finally settle is not obvious, as there’s no reason to think the end of these advancements is in sight. If we want to know what the final definition will be, the question to ask is ‘How badly decayed does a human body have to be before a person could not, even in-principle, no matter the technology, be restored to health?’ This chapter is going to answer that question and provide a definition of death that applies at that limit. Let’s start by considering what it currently takes for someone to be formally considered dead.
(Mis)Pronouncing death
First of all, it’s worth acknowledging that, when considering one’s own life in isolation, a rigid definition of death isn’t necessarily all that useful. While most people are concerned about their own survival, they’re generally very unconcerned about the possibility that their survival may be ambiguous to them. Thought experiments and science fiction aside, knowing you haven’t died because you’re still alive is a perfectly workable definition.
As is so often the case, things become more complicated when other people are involved. People are not just isolated individuals, we come with tangles of responsibilities, obligations, debts, and other relationships. For example, meet Alex. She works as an engineer, has a spouse named Blake, and owns a house. It’s not something we often like to consider, but what would happen were Alex to die? As a society of government agencies, unions, and mortgage brokers, we want to be very clear on the conditions under which Blake’s aspirations for their joint life should end, the mutual obligations between Alex and her employer cease, and when her claims to property can be disregarded. As well as being legally significant, defining these conditions is of considerable emotional and practical importance. It marks when Alex’s friends and family should mourn her just as much as when her property should be distributed to inheritors. While an individual themself has no need to know when they are dead, the others in their community certainly do.
Certain social statuses of individuals, like marriage and employment, are so consequential they are formalized by law. As such, let’s consider the legal definition of death. There is a reasonable level of consistency in this across different jurisdictions.3–5 Most commonly, a person is defined as dead if either or both of the following applies to their body:
1. Irreversible cessation of blood circulation.
2. Irreversible cessation of all functions of the brain, including the brainstem.
Considering we live in the age of cardiopulmonary bypass and extracorporeal membrane oxygenation machines, which can keep your blood circulating with the ease of a pool pump keeping a jacuzzi’s bubbles flowing, it’s immediately apparent that it will not always be straightforward to apply this definition.[4] For this reason, laws typically include a statement such as ‘a determination of death must be made in accordance with accepted medical standards’. While pragmatic, this combination of underdefined law and deference to doctors is the foothill to a towering mountain of definitional problems.
There are at least two issues with the legal definition of death. The first is that what counts as ‘irreversible cessation’ is as much dependent on medical technology as it is on the damage to a person’s body. Declaring an injured person dead or alive based on what medical equipment is available is a bit like saying perfectly edible food is already off because there’s no refrigerator nearby. In other words, if we’re defining death by properties other than those intrinsic to a person, we’re on shaky philosophical ground. The second concern is the requirement that ‘all’ functions of the brain are irreversibly lost before a patient is declared dead. It turns out that this requirement is out of touch with both the beliefs and actions of doctors. While these issues can be safely ignored in the vast majority of deaths, we’ll soon see exceptions illustrating how our current definitions of death are problematic.
In response to the decreasing emphasis placed on blood circulation with the advent of artificial cardiorespiratory technology, modern medicine became more concerned with defining death based on the loss of brain functions, commonly termed brain death. Later, we’ll see how current and developing technology is increasingly rendering brain death as obsolete a concept as cardiopulmonary bypass did for heart death. But, before even coming to how the functions of natural brain tissue could be replaced with prosthetics, it’s worth focusing on how doctors already ignore the legal requirement that death requires the loss of all brain functions.
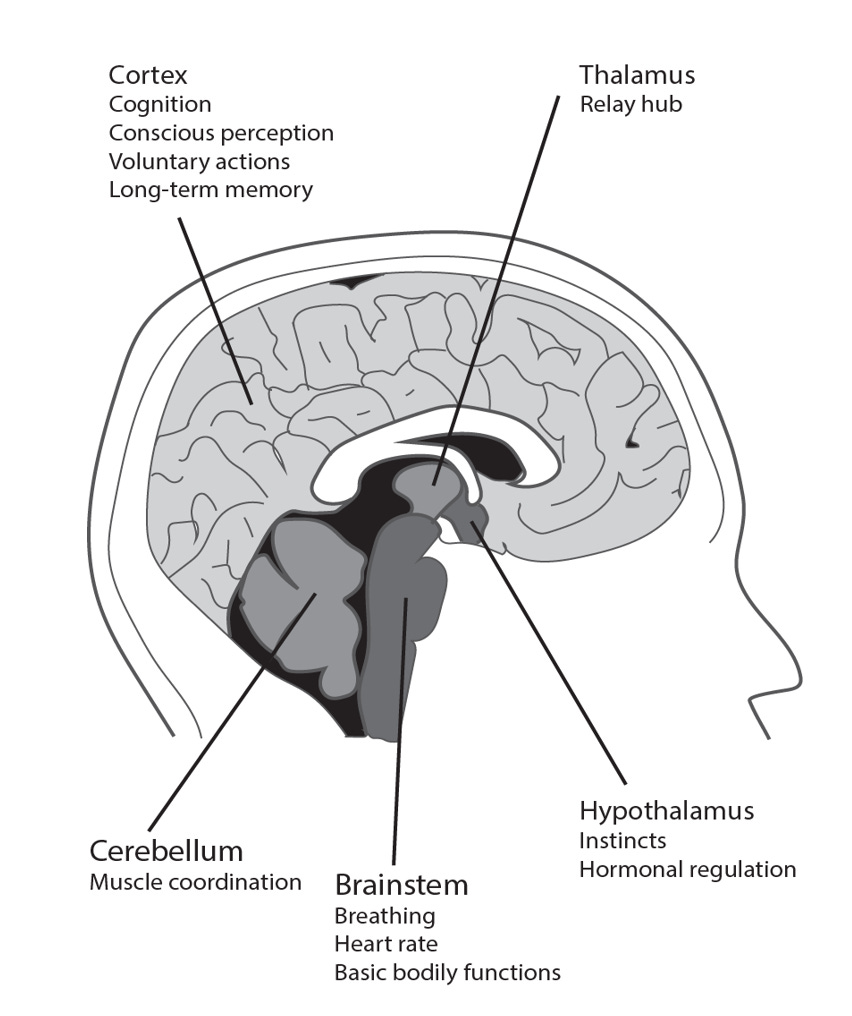
For example, consider the hypothalamus. A small, nugget-shaped region at the base of the brain, it is involved in regulating instincts, hormones, and many other basic bodily functions (Fig. 3). Contrary to the requirements of the second legal definition of death, the hypothalamus is often still mostly working in patients otherwise declared brain dead.[5],6. While not at all compatible with the legal notion of ‘whole-brain’ death, this is quietly but consistently ignored by the medical community. Even stranger, there is other evidence suggesting there are often isolated ‘islands’ of preserved neural tissue in brain-dead patients, even though most of the rest of the brain has ceased functioning.7
Figure 3. A side-on view of the middle of the brain.
While it doesn’t affect day-to-day practice, the medical profession is well aware of the gap between the written letter of the law and actual implementation. Calls to resolve this have been made in prestigious journals, though this has had little impact.8 Despite the tension, doctors issue tens of thousands of death certificates per day without worrying they are falsely pronouncing patients dead. Why are they so unconcerned? Because routine diagnostics can uncover sufficiently extensive brain damage indicating that patients have no hope of functional recovery, even if strictly speaking they do not meet the criteria for whole-brain death.
The following tests for brain function are generally applied, though with some variation between jurisdictions.9 No proper examination is necessary if it is obvious that there is no possible brain function remaining, such as when a person’s body has been incinerated, pulverised, or is clearly rotting. Otherwise, a combination of diagnostics for residual cardiorespiratory and neurological function are performed. A doctor will check for signs of breathing or cardiac activity.[6] In addition, they will check for responsiveness to pain by pushing down on the patient’s forehead, and for a pupillary response by shining a light into their eyes. If none of these signs are present, the patient can be declared dead.
These simple tests are taken to be accurate diagnostics of death because they assess the function of the brainstem, a brain region critical for normal functioning. The brainstem is an evolutionarily primitive anatomical structure resembling the stem of a plant, connecting the spinal cord at its roots to the rest of the brain at its branches. It regulates certain basic functions such as breathing, heart rate, and the overall wakefulness of the rest of the brain. Damage to the entire brainstem necessarily entails permanent loss of consciousness and breathing, so checking for brainstem death is a convenient shortcut for assessing whole-brain death. The pupil shrinkage that doctors are looking for is useful because the clusters of neurons that control constriction are present in the brainstem, so a persistent absence of shrinking pupils is a pretty clear indication the patient won’t ever be coming to again. The everyday bedside diagnostics described above are normally sufficient to declare a patient dead because brainstem death suggests widespread, irreversible cessation of important brain functions.
Yet, in the same way that doctors dismiss ongoing hypothalamic functions as signs of life in patients with brainstem damage, there are calls by some philosophers to recognize certain patients as dead even if some brainstem function is maintained. Sometimes much of the brain can be destroyed while sparing the brainstem, meaning the corresponding body may continue spontaneously breathing while doing little else. The higher-brain view of death, in contrast to whole-brain, claims that, in circumstances such as these, whether a person’s body has a gag reflex is as irrelevant to whether they’re alive as whether their fingernails are growing.10 Advocates argue that if a person’s reasoning functions are gone, their memories destroyed, with no self-awareness remaining, and in fact no capacity to experience anything at all, then the person is dead. Because evidence suggests that higher-brain structures such as the cortex support these functions, the argument goes, cortical destruction alone is enough to entail death.
So far, no jurisdiction nor medical association has endorsed the higher-brain concept of death, even if actual medical practice suggests implicit support for the idea. There are several reasons why this is the case. The largest is that many people are disturbed by the idea that a spontaneously breathing human could be dead.[7] Another is that it is much more difficult to design useful diagnostic tools for higher-brain death than brainstem death.[8] A further issue is that there are no generally agreed-upon criteria for determining the degree of higher-brain damage required for irreversible loss of personhood. Without a widely accepted theory of consciousness it is difficult to tell the difference between a patient whom brain damage has left irreversibly unconscious and a patient possessing severely degraded consciousness.
Additionally, in the absence of similarly clear markers as in brainstem death, there are fears that criteria based on higher-brain death may erroneously mark patients as dead who may one day recover consciousness. Unless a better understanding of the exact brain mechanisms that underlie consciousness is found, or disregard for spontaneous breathing becomes widespread, the higher-brain concept is unlikely to become broadly adopted.
This decision to require destruction of the brainstem, rather than just the cortex, is thus more of a pragmatic choice than a rigorously defensible philosophical position. Doctors have been tasked with fulfilling the social need to identify when individuals die, and have chosen uncontroversial and conservative criteria to mark the boundary. Their aim is to declare dead only those with absolutely no hope of regaining consciousness, while being sensitive to differing cultural and religious views. They are also acutely aware that people are much more disturbed by falsely declaring living patients as dead than vice versa. As a result, doctors err closer to the whole- than higher-brain concept of death. In doing so, they take the safer route of declaring dead only those with such extensive brain damage that their irreversible loss of consciousness is uncontroversial.
This conservative choice is still controversial, though, as it may be killing more patients than it saves. Failure to declare patients with higher-brain death dead can mean that other, definitively conscious patients die who would otherwise live. Current organ transplantation practice follows the dead donor rule, which states that a person must be dead before life-prolonging organs can be procured from them. Some think it is deeply unethical that a patient with higher-brain death, who will never regain consciousness, is kept in care while their organs could be used to extend the life of one or more active, conscious, hopeful patients. Others think that taking donations from such patients would be an unconscionable act of murder, regardless of the positive consequences it may have. Another take is that even if doctors broadly agreed that higher-brain death should be considered death proper, this shouldn’t be acted upon without clear public support. This comes from a worry that more organs would be lost from people withdrawing consent to be potential organ donors, due to fear of being wrongfully pronounced dead, than would be gained from the small number of cases of higher-brain death without brainstem death. The debate on this is not settled, though there are no signs any jurisdictions are considering shifting from the whole-brain definition anytime soon.
Regardless, all these definitions of death are unsatisfying if we want to know when a person is dead in principle, even in the face of considerably better medicine than we have today. None of the current definitions really try to address what it is for brain damage to be truly irreversible. To know where this point-of-no-return is, we need to examine how brain damage occurs in a dying brain at a deeper level than just loss of whole brain regions. I’m sorry, this is going to be even less pleasant to think about than the chapter has already been thus far. But if we want to know where the limit is, we need to look at exactly what would be happening in your brain if you were imminently dying.
From cardiac arrest to brain death: A timeline of dying
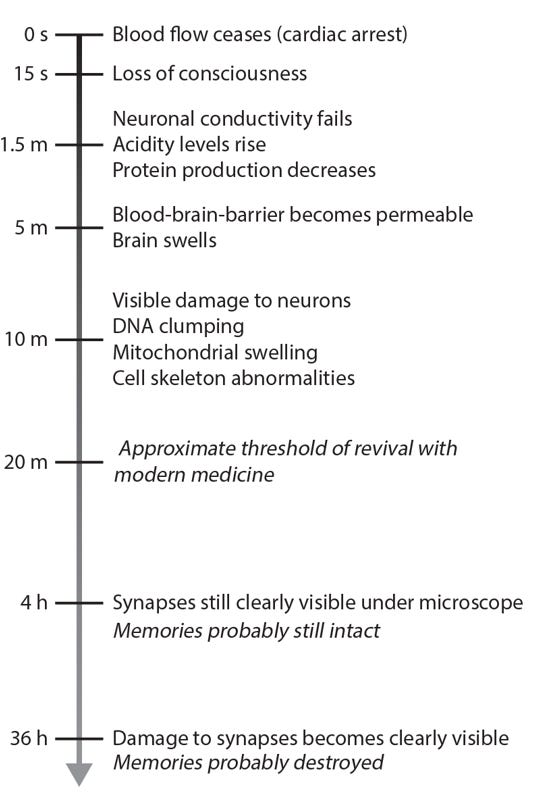
Imagine Alex is at home sitting on the couch when she suffers an untimely cardiac arrest. Her heart is no longer pumping blood around her body, so her organs are suddenly starved of life-sustaining nutrients and oxygen. Poor Alex is now rapidly dying, her cells screaming for food and choking on their own waste products. Prompt medical attention could potentially save her. The question is, how long does Alex have before she is irreversibly dead (Fig. 4)?
Figure 4. The timeline of changes to the brain following cardiac arrest.
About fifteen seconds after her heart stops beating, Alex’s subjective experience will dissolve into unconsciousness.[9],11 This is so quick because the brain is disproportionately energy hungry, consuming 20 per cent of the body’s energy, yet has essentially no reserves. Specifically, Alex’s neurons are no longer able to regulate the release of neurotransmitters, the chemicals neurons use to send signals to each other, as this process is particularly energy intensive.12,13 Without precise neurotransmitter release there can be no coordination of activity between neurons, a prerequisite of consciousness according to any scientific theory. Scalp recordings of her brain waves would correspondingly show a complete loss of cortical activity. If Alex does not receive medical attention soon her unconsciousness will become permanent. Things may seem dire, but at this stage there is still hope.
At about the ninety-second mark, Alex’s neurons will run out of energy and become unable to send electrical signals along the branching dendrites and axons of their cell bodies.14 In essence, this is similar to a phone line losing power – the line is still there, but it no longer functions.[10] At this point her neurons are no longer capable of information processing even if they were receiving coherent neurotransmitter signals. Neuronal conductivity failure due to depleted energy supplies marks the beginning of the danger zone for Alex.
From here on out, her starving neurons will start to destroy themselves in their panic and desperation.15 Molecular pumps that control the flow of ions like sodium, potassium, and calcium start to fail, flooding some areas of the neurons with ion levels they cannot handle. A particularly bad result of this is that abnormally high internal concentrations of calcium lead to dysregulation of mitochondria, the energy-producing organelles of the cell. The carbon dioxide they generate as a waste product cannot be removed by the blood and instead accumulates as acid.[11] Increasing acidity damages the proteins that make up the existing molecular machinery, while the lack of cellular energy means new proteins stop being produced. By the ten-minute mark, abnormal DNA clumping, mitochondrial swelling, and damage to the neuron’s internal skeleton are apparent.16 As the damage accumulates, Alex’s chances of ever making a functional recovery dwindle smaller and smaller.
Without medical attention, Alex’s chances of successful resuscitation are dropping at roughly 5 per cent per minute.17 As time goes on, Alex’s brain becomes so vulnerable that ironically even restarting her blood flow will invite damage. In part, this is because by the five-minute mark, the protective blood–brain barrier has partially broken down. This barrier normally exists to shield the brain from infection or dangerous chemicals that might be carried by the blood. Breaches in this cerebral sea-wall not only let fluid in, resulting in dangerous swelling, but also mean that the return of blood flow will allow inflammatory and toxic materials to enter her brain.18 At this point, Alex’s life is not so much hanging in the balance as rolling rapidly towards the edge of the abyss.
Probably within five to twenty minutes following cardiac arrest, Alex passes the threshold at which current medicine is able to restore her to consciousness.19 If nobody finds and attempts to resuscitate her, she will reach the whole-brain definition of death once her brainstem is sufficiently damaged. But even if she is found and cardiopulmonary resuscitation (CPR) started early enough to prevent irreversible loss of spontaneous breathing, she may never regain consciousness.20
If she is resuscitated just before the transition to whole-brain death, her body may survive in a coma. In this state, enough brainstem neurons survive to command spontaneous breathing, but that’s about all the behaviour her nervous system can muster.
Were Alex to be resuscitated a little earlier, she may instead end up in a persistent vegetative state.21 In this case, a little bit more of the brainstem has survived, and Alex displays signs of a sleep-wake cycle as well as spontaneous breathing. This means that she may open and close her eyes for periods of the day, and even perform eye movements, but without showing any responsiveness or environmental awareness.22 Unintuitively, perhaps, this is no clear indicator that Alex is somehow conscious. Sleep is such a primitive neurological function that it can even be found in animals without brains, such as jellyfish and worms.23 Sadly, all Alex’s sleep-wake cycle indicates is the survival of a simple brainstem circuit akin to an alarm clock, nothing more.
Resuscitated a bit earlier still and it becomes hard to tell whether Alex returns to consciousness or not. A minimally conscious state can occur if some of her cortex is spared in addition to her brainstem. In this case Alex would still show heavily impaired behaviour, but may be able to provide very basic responses, such as occasional eye movements in response to a yes/no question. Brain scans would show greatly reduced activity relative to a neurotypical person, but still significantly more than if she were in a comatose or vegetative state.
From here on, earlier resuscitation means increasingly better clinical outcomes. Patients may suffer ‘only’ from memory loss and other cognitive impairments, while a lucky few may not show detectable impairments.24,25 If CPR and resuscitation is commenced early enough, Alex may even make a full recovery.
But even if no-one finds her, it's worth noting that the moment Alex slips past modern medicine’s point of no return and suffers ‘irreversible’ damage is not indicated by a definitive change in the structure of her brain. On the one hand, her neurons would have stopped communicating long before this time, having been silent for many minutes now. On the other hand, much of the important structure of her brain will continue to exist for some time. In particular, the synaptic connections between neurons that store Alex’s memories may well still be intact. Some mild swelling of the neurons is apparent five minutes after cardiac arrest, but not enough to destroy the synapses.[12],26 In fact, Alex’s synapses are still clearly identifiable at least four hours after her blood flow has ceased, and often don’t become difficult to make out until almost a full day has passed.27,28 Not enough research has yet been done to determine the exact rate of synaptic degradation, and it’s possible that molecular-level damage occurs to the synapses earlier than they become visibly damaged under a microscope.[13] But it certainly seems plausible that Alex’s memories still exist for hours after she draws her final breath. While modern medical science is unable to repair the damage incurred from twenty minutes of neural asphyxiation, it’s not at all inconceivable that better technology could push this window further out.
If future medicine could push the point of irreversibility from twenty to forty minutes, or further still, how are we to decide when Alex has died? Does it matter if we push this limit back through keeping the current neurons intact longer, or is replacing them fine? As one of the best-known defenders of the whole-brain view of death claimed in 1998, ‘the idea of a mechanical, electrical, or synthetic brain […] would force us to alter completely our concepts of death and personhood’.29 As we will soon observe, this crisis in definition entailed by biotechnological progress is already at our doorstep. Once we take a look at the facts, we’ll see why a philosophically rigorous replacement for current death definitions is needed before this technological trend develops any further…
‘The Future Loves You: How and Why We Should Abolish Death’. Available now in hardcover, audiobook, eBook.
[1] Actually, even back then this wasn’t always quite true, as people would occasionally be pronounced dead only to regain signs of life later. Fears of being erroneously pronounced dead were great enough that in 1896 the London Association for the Prevention of Premature Burial was founded to try and improve procedures for doctors checking for signs of life prior to burial, and to ensure warning devices were placed in coffins that could be used in case these checks failed.
[2] Now unfortunately well-known due to the COVID-19 pandemic.
[3] I’m fairly certain that was the original intent behind their design, but note that they would have been inspired by the earlier ‘iron lungs’, which were used to help polio patients during recovery from paralysis.
[4] In practice the process of keeping someone’s blood flowing is probably trickier than that of a pool pump, but the principle is the same. You understand the point.
[5] When they’re left on cardiorespiratory support.
[6] As noted previously, this is more because if cardiorespiratory functions have ceased then brain functions will stop shortly thereafter, not because blood circulation alone is taken to be important. If that were the case, every brain-dead patient could be ‘revived’ by hooking them up to a cardiopulmonary bypass machine.
[7] The American medico-legal case of Karen Ann Quinlan is a paradigmatic example. In 1975, she entered a persistent vegetative state at the age of twenty-one, after she stopped breathing for twenty minutes due to consuming alcohol and benzodiazepines. Imaging showed signs of irreversible higher-brain damage, and she was eventually taken off a ventilator after some legal controversy. Though her body continued breathing due to an intact brainstem and ‘lived’ for another nine years, she never regained signs of consciousness.
[8] In particular, doctors are worried about missing cases of locked-in syndrome, where a patient is completely paralysed but still conscious. Sophisticated behavioural tasks and brain scans are able to show evidence of this in a small number of brain-injury patients.
[9] Probably at this stage, and definitely within one minute, Alex will also stop breathing. This doesn’t really matter, as without blood circulation breathing is pointless.
[10] Neurons are unable to conduct electrical signals from this point onwards because of the loss of power to their ion pumps. Under normal conditions these pumps ensure unequal concentrations of sodium, potassium, and calcium ions are maintained inside and outside the neurons, which is necessary for electrical signalling. When cellular energy sources are depleted, these pumps cease working and ion concentrations equalize between the inside and outside of the neurons. The loss of the ion-concentration gradient results in the loss of a voltage difference across the surface of the cell, and with it the ability to conduct electrical signals.
[11] It’s actually more complicated than this and includes steps involving bicarbonate buffers, lactic acid, and other enzymes, but this will do for now. Sorry.
[12] The review cited here by Krassner and colleagues is the most comprehensive review of this literature that I’m aware of.
[13] It’s equally possible that the information in them actually lasts even longer, and that the visible damage can easily be compensated for through sophisticated analysis techniques.



Excellent, as usual. It looks like the footnotes got cut off...
Information death is probably the best definition of death conceivable, in my opinion. However, I believe it is possible to consider that there may be enough residual biological information in the human brain after 36 hours of warm ischemia to allow for an analysis of the remaining synaptic matrix using future algorithms and a reconstruction of personal identity.